Pacemakers
Pacemakers can be temporary or permanent. Temporary are used in emergencies and usually used only a few days at most.
What does a pacemaker do to an EKG rhythm strip?
it creates pacer spikes.
a. Types of Pacing Response- Each pacer has settings programmed into it and is either triggered, inhibited, or both.
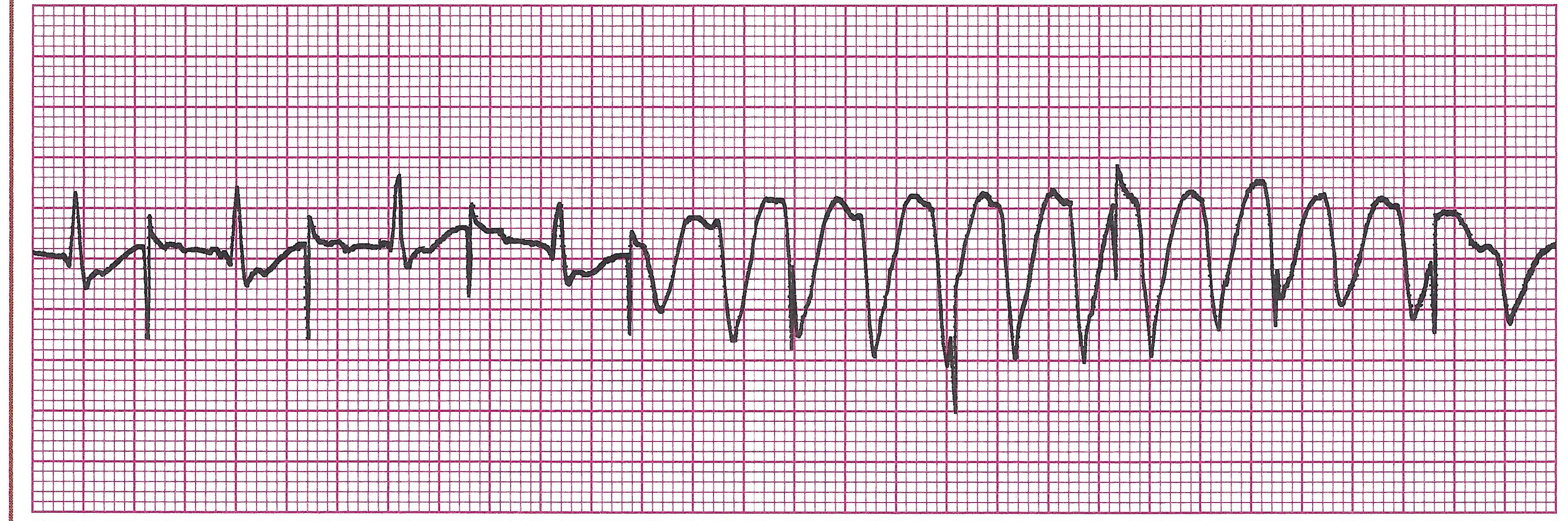
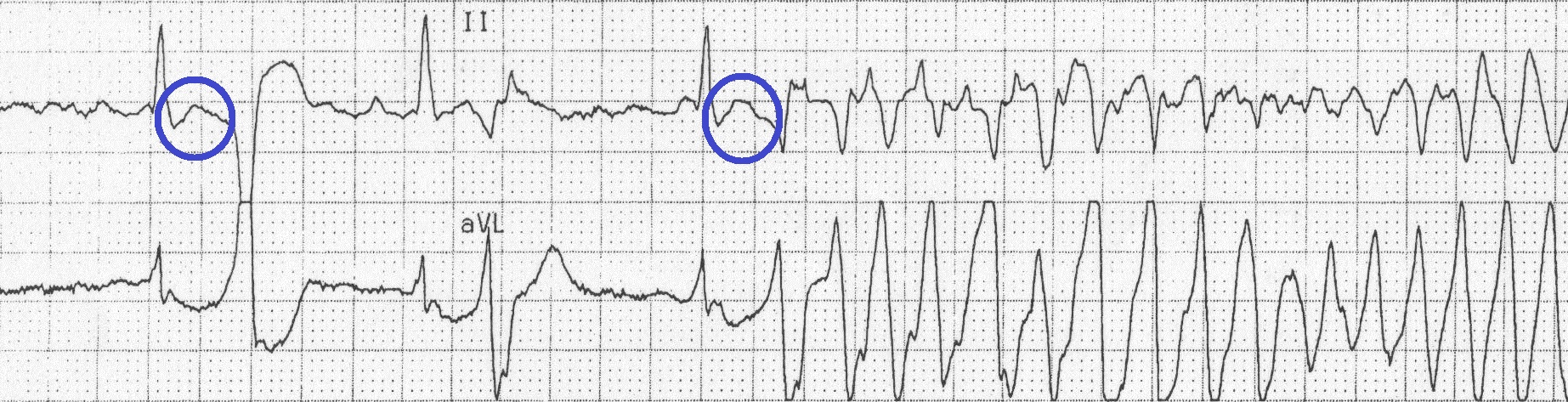
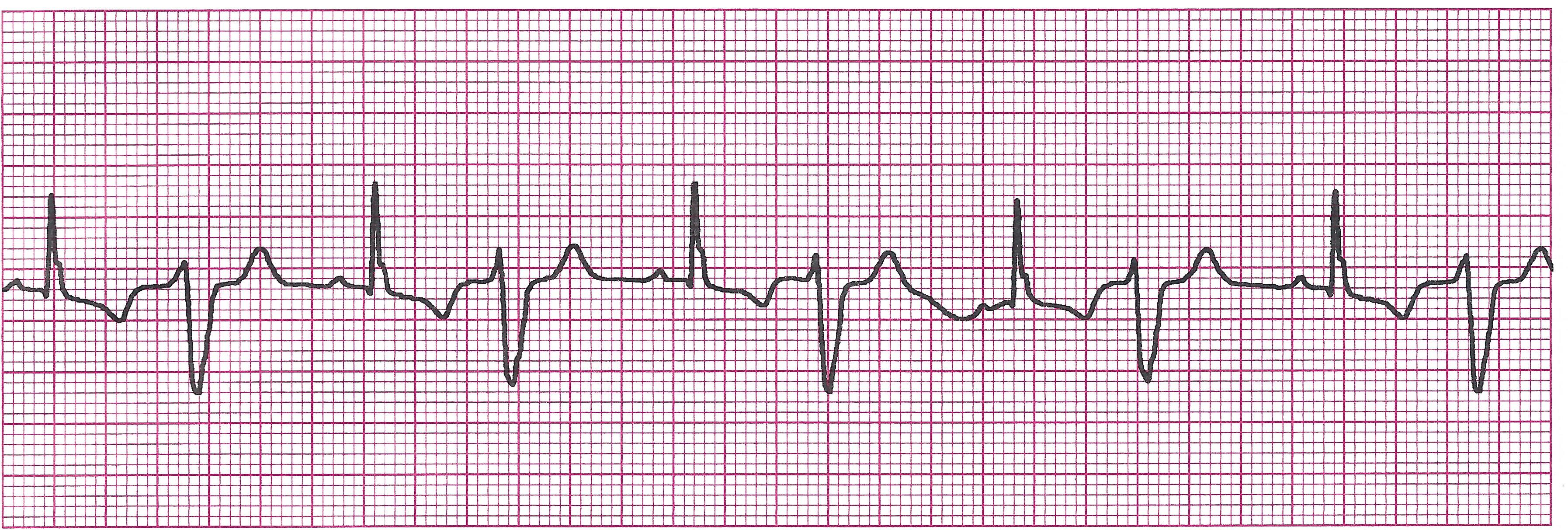
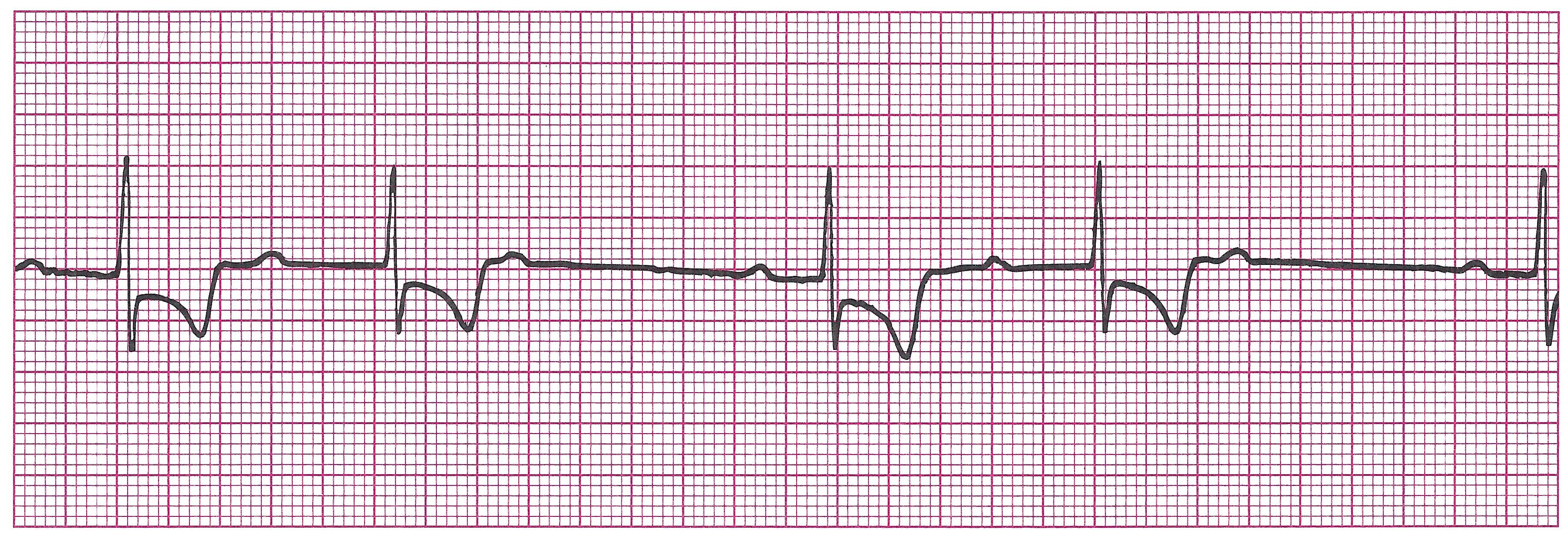
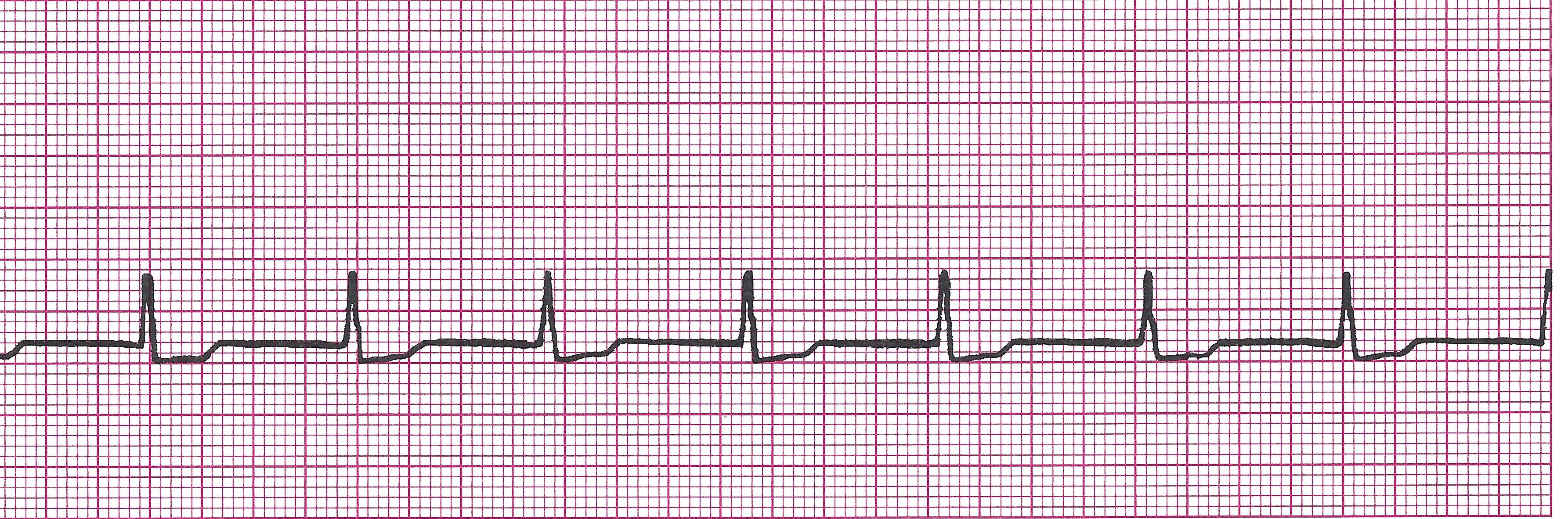
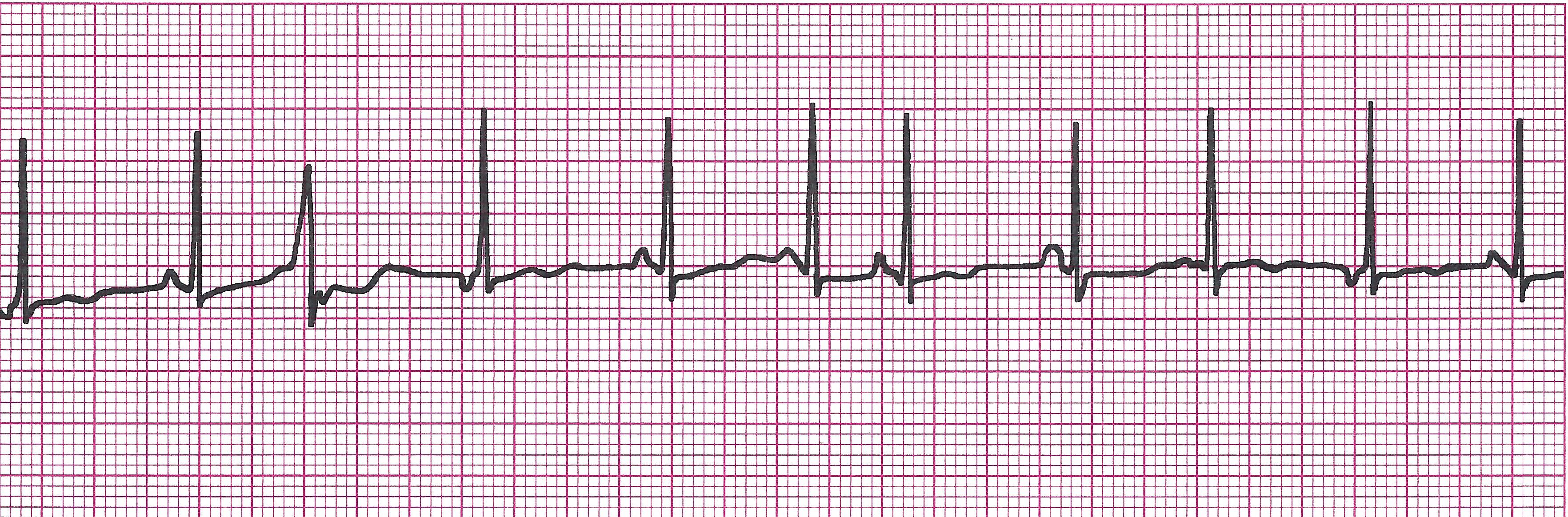
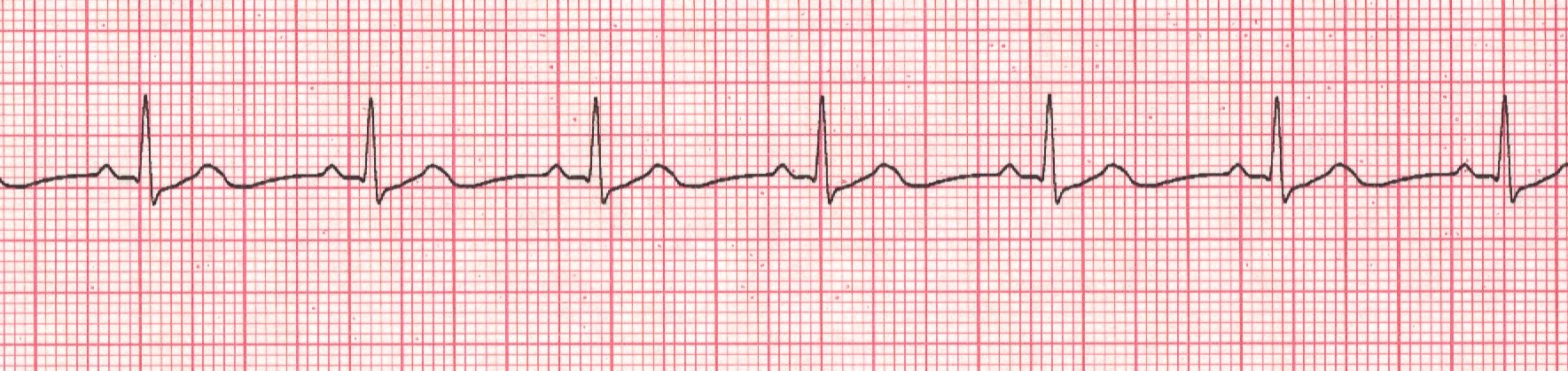
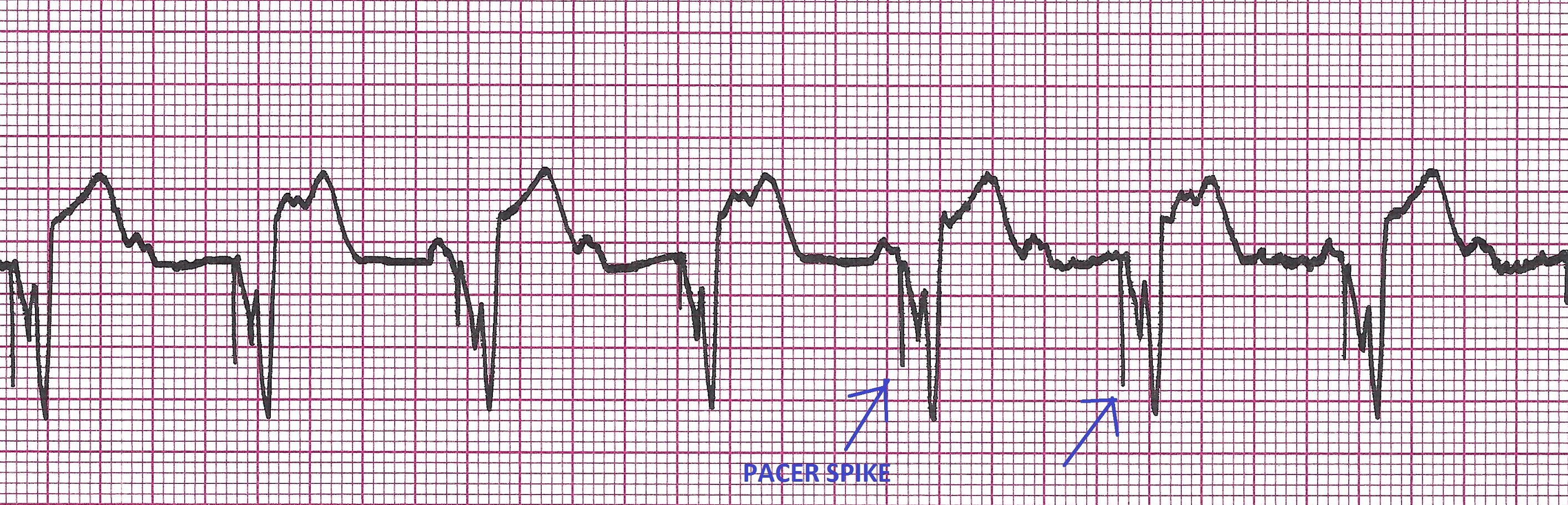
1) Triggered- Fixed rate. Fires according to a predetermined program regardless of patient’s underlying heart rate or rhythm. (i.e. pacer is programmed to send 75 impulses to the ventricles every minute regardless of what the atria are doing as in the strip below).
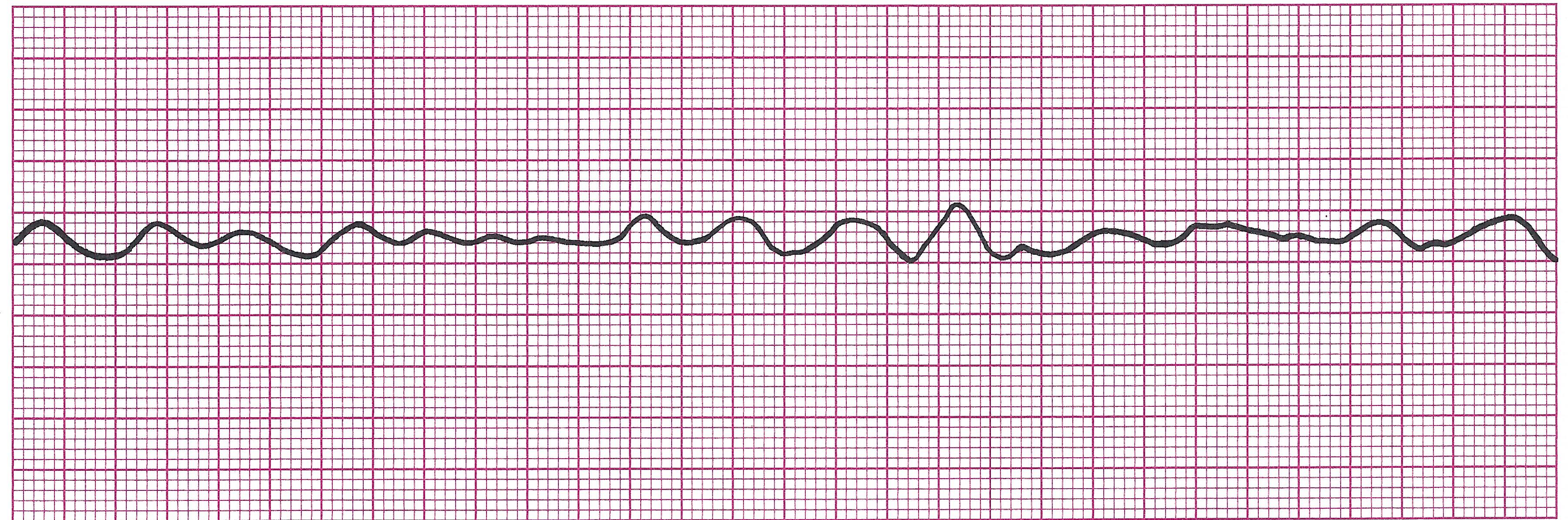
Example EKG strip with Triggered pacing

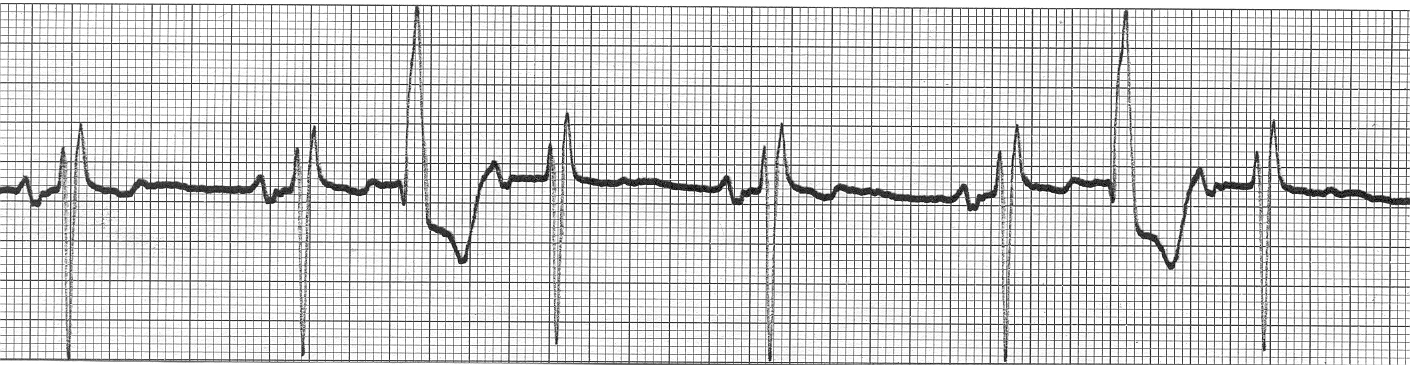
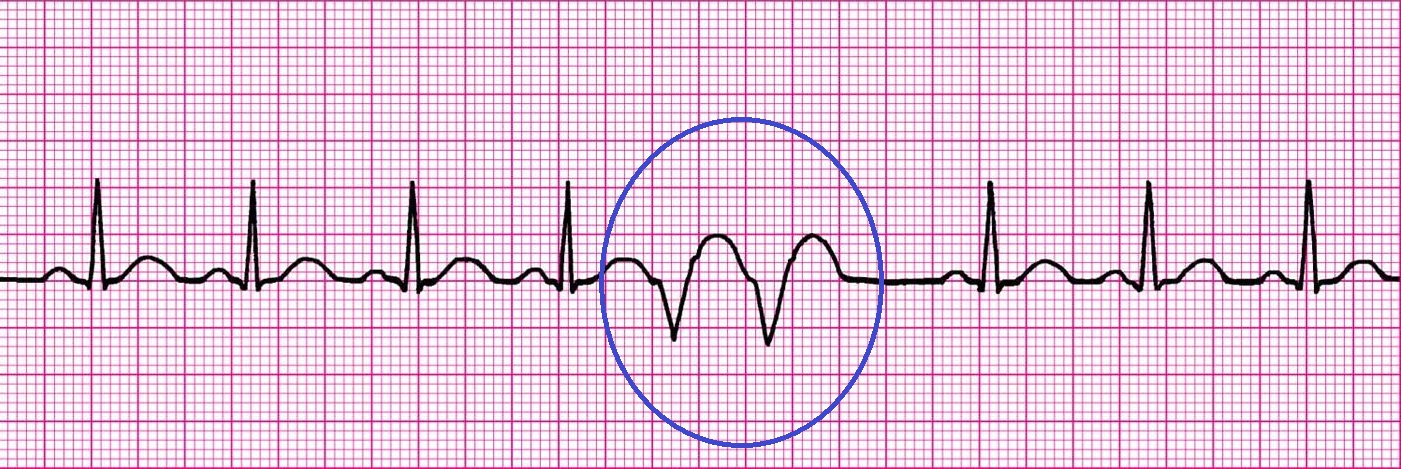
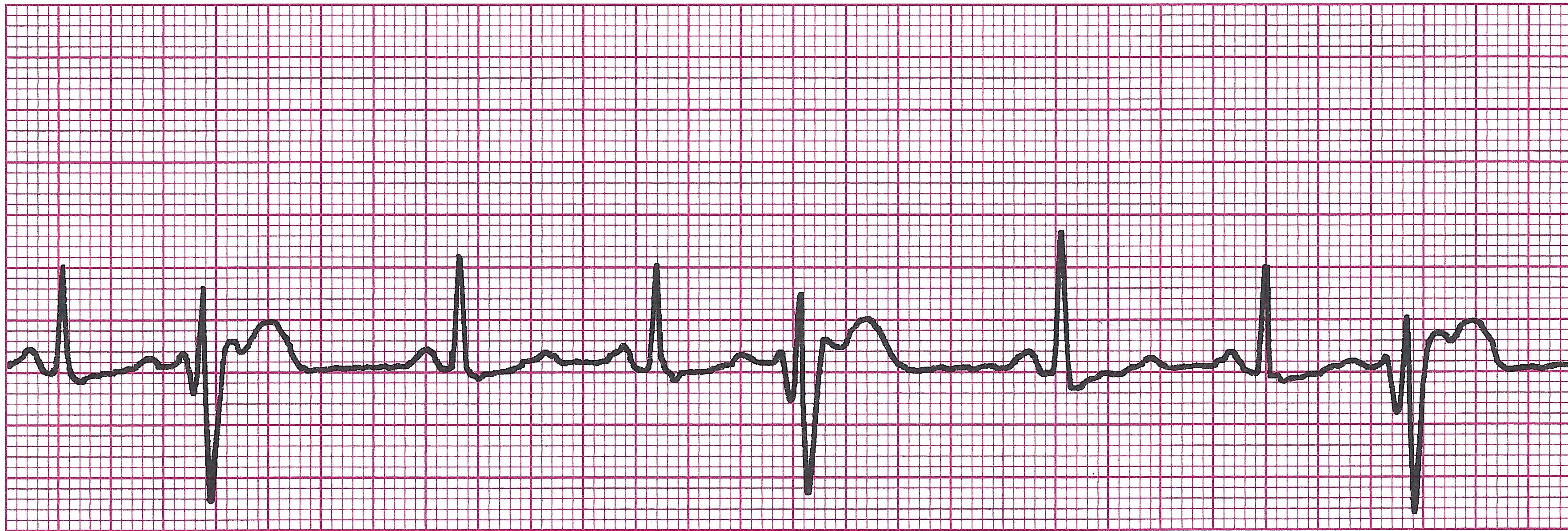
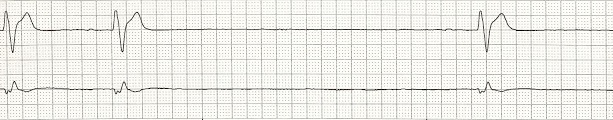
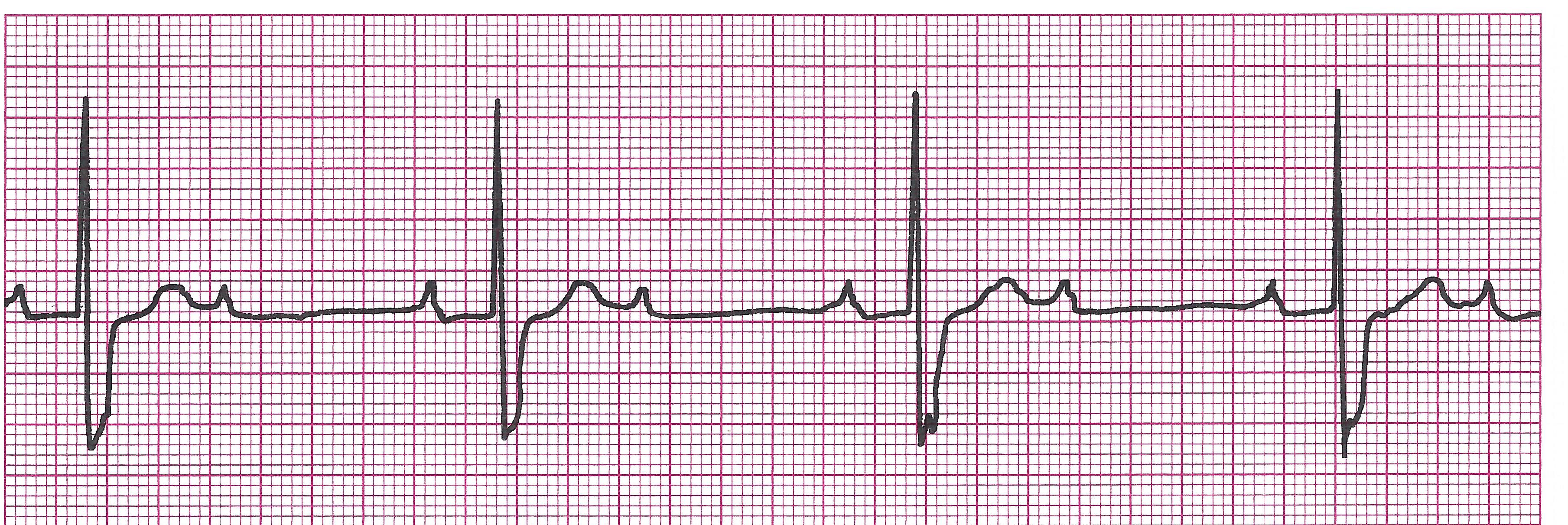
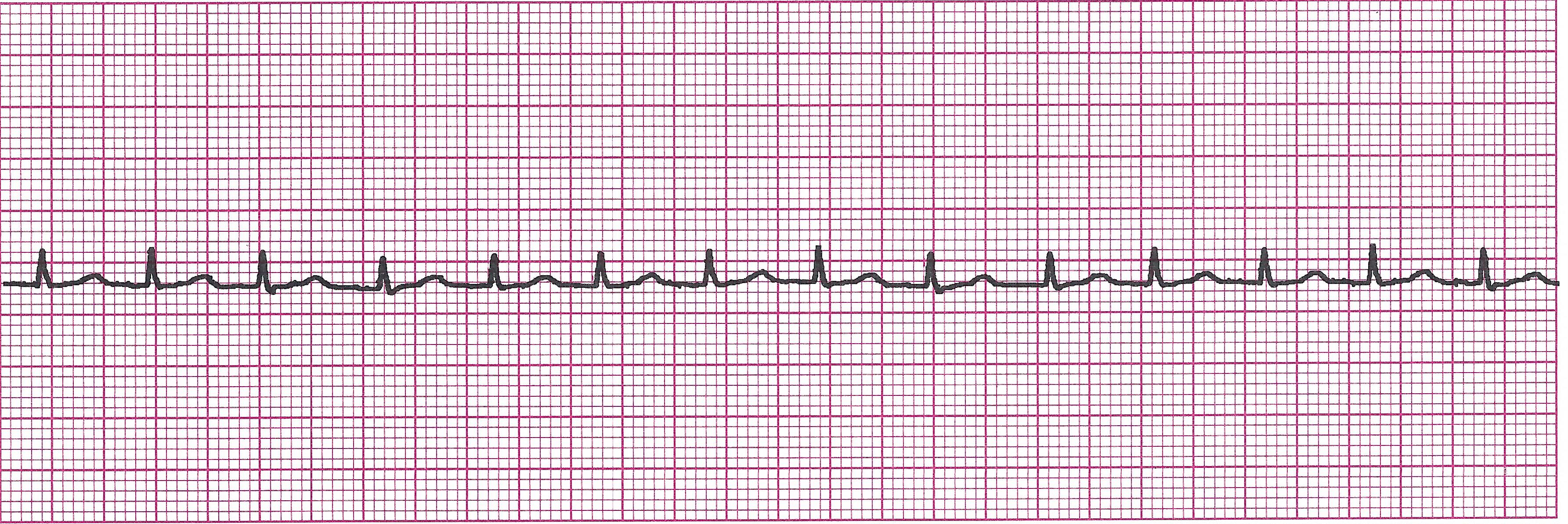
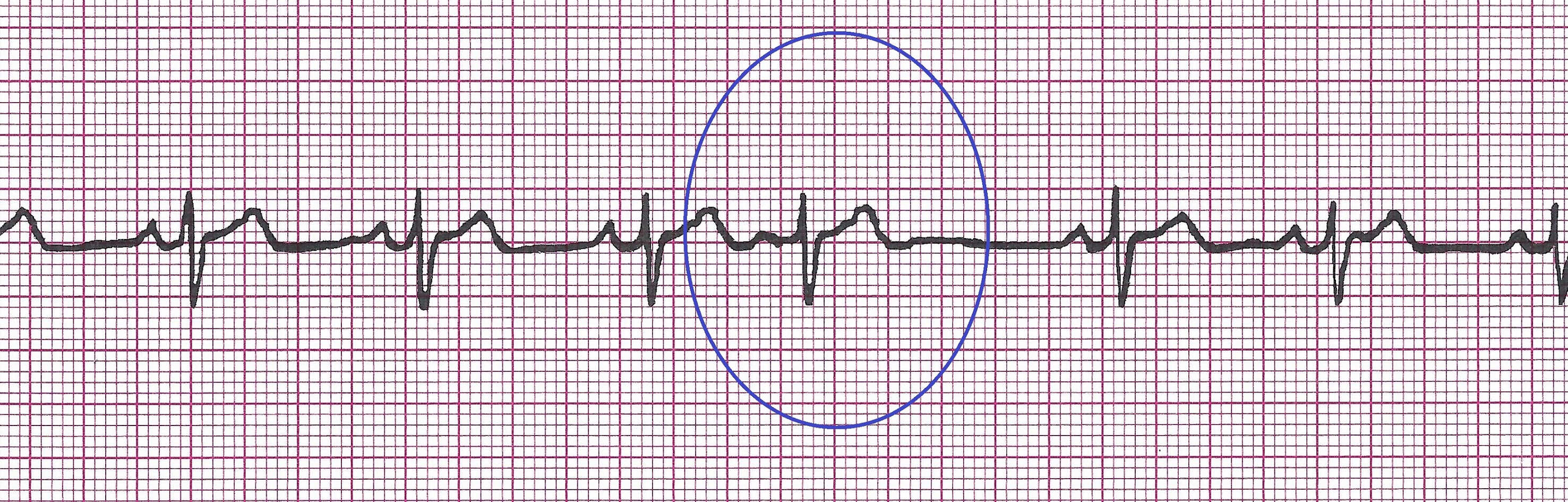
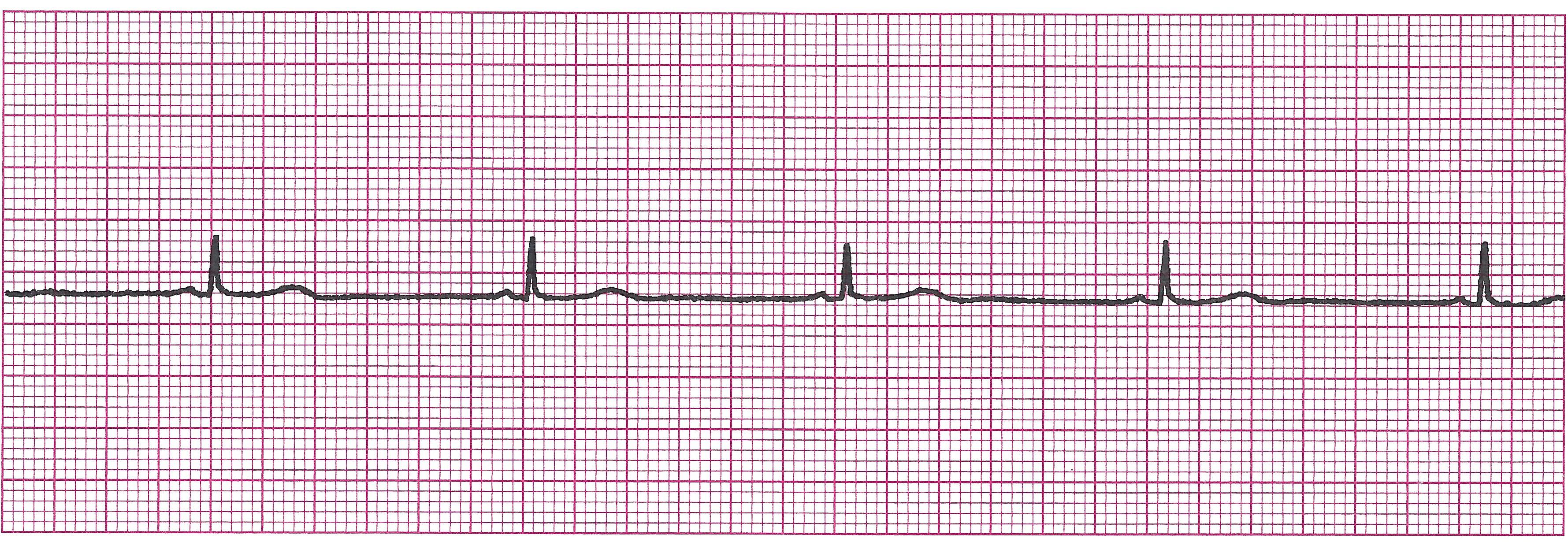
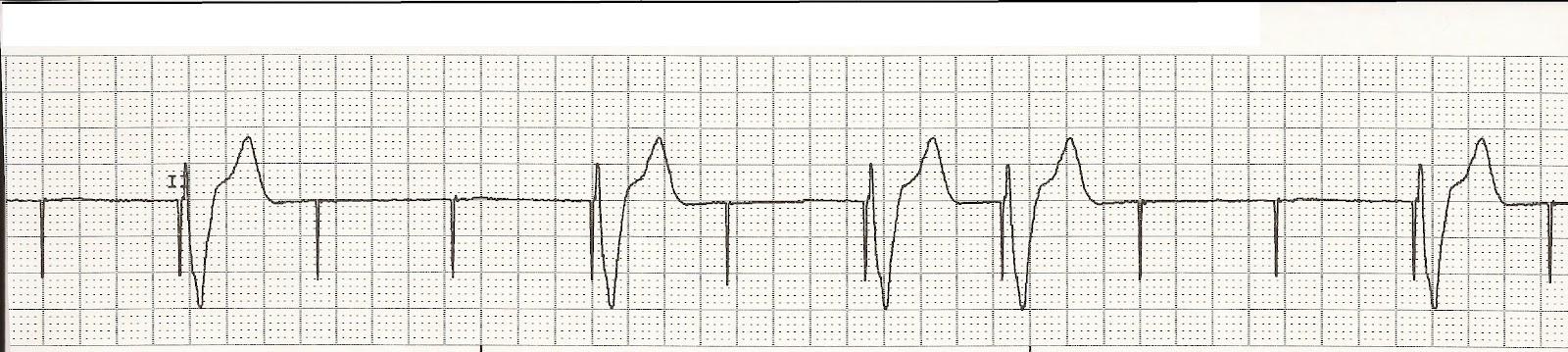
2) Inhibited- Fires only when needed. Senses patient’s own rhythm and inhibits its impulse until needed (i.e. the ventricle or atria stop beating or are beating too slow, etc). In the strip below, you can see the pacer only kicks in after the patient's ventricles fail to beat.
Example EKG strip with Inhibited pacing

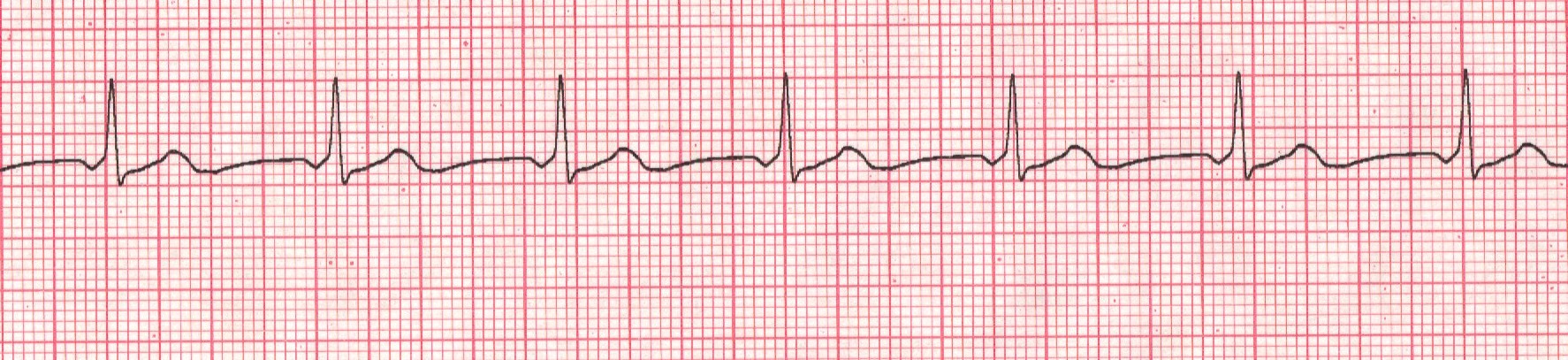
Can be both: Triggered atrial, (this means the pacer sends an impulse to the atria regardless of how the atria are beating) and inhibited ventricular (this means it senses ventricular beats and fires only when ventricles need it to).
b. Common Kinds of Inhibited Pacers
1) Single chamber- Senses and stimulates either atria or ventricles but not both
2) Dual chamber-Works on both chambers simultaneously. Most common is DDD-Dual pacing for both chambers, Dual chamber activity sensing, and Dual response (triggering and inhibition).
c. Assessment
1) Things to assess
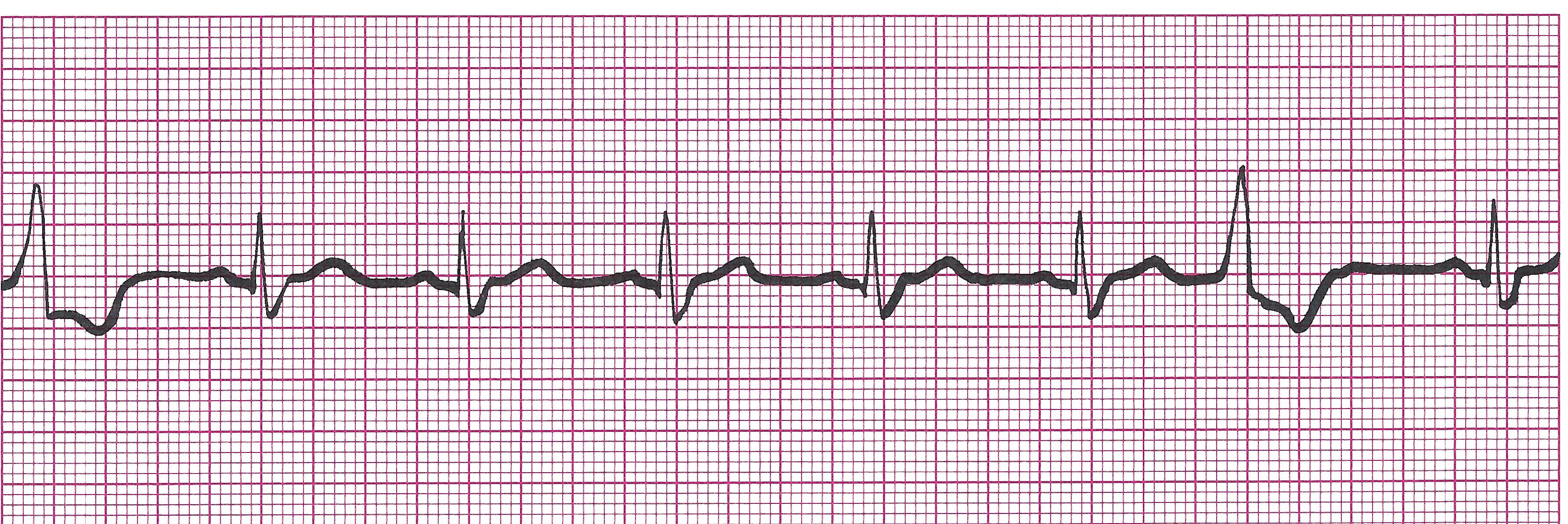
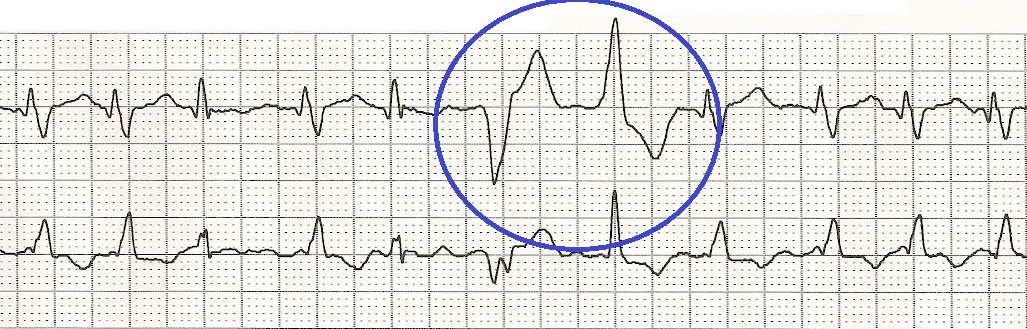
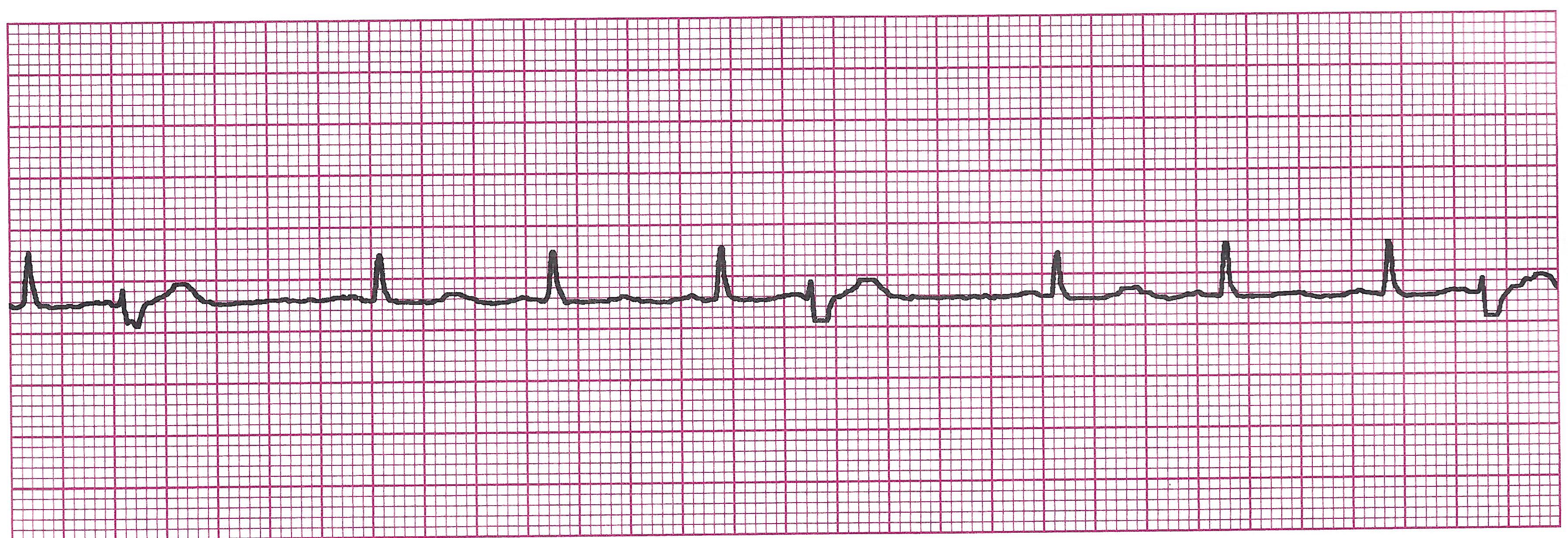
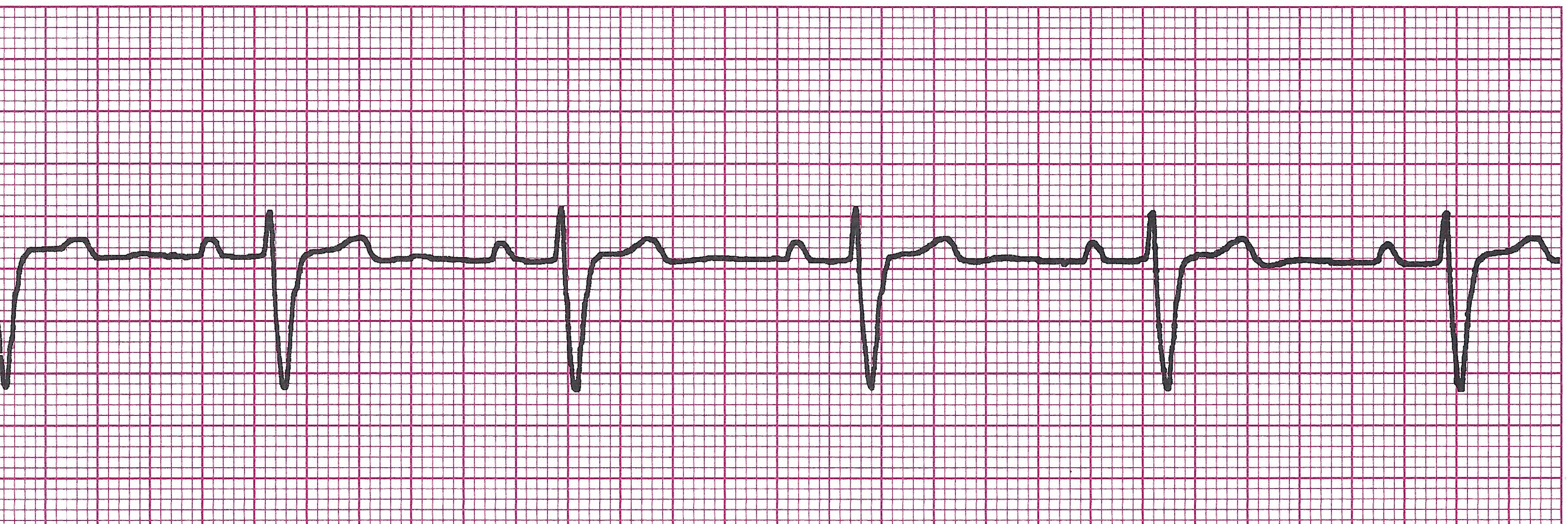
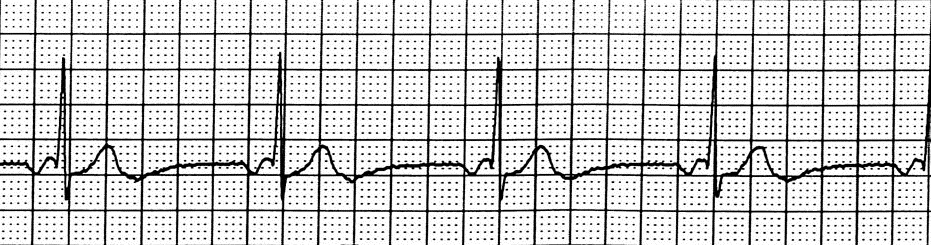
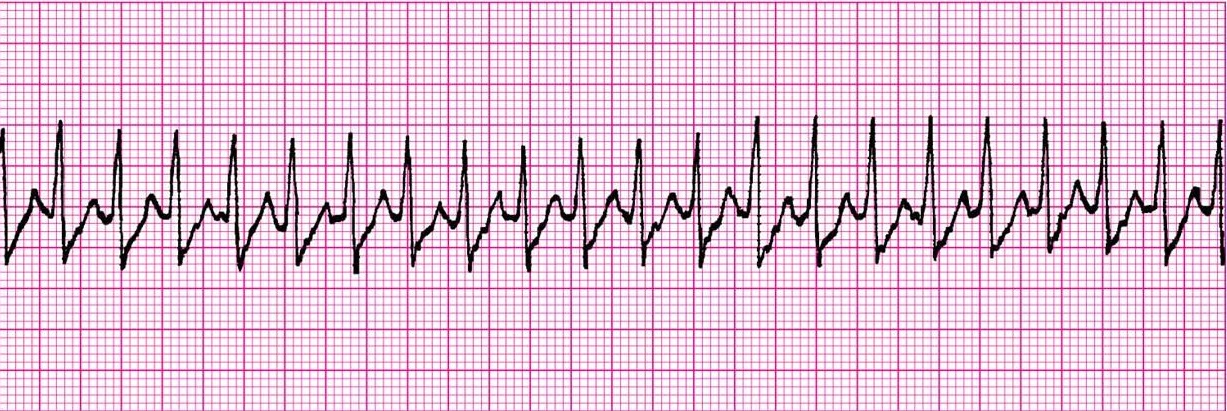
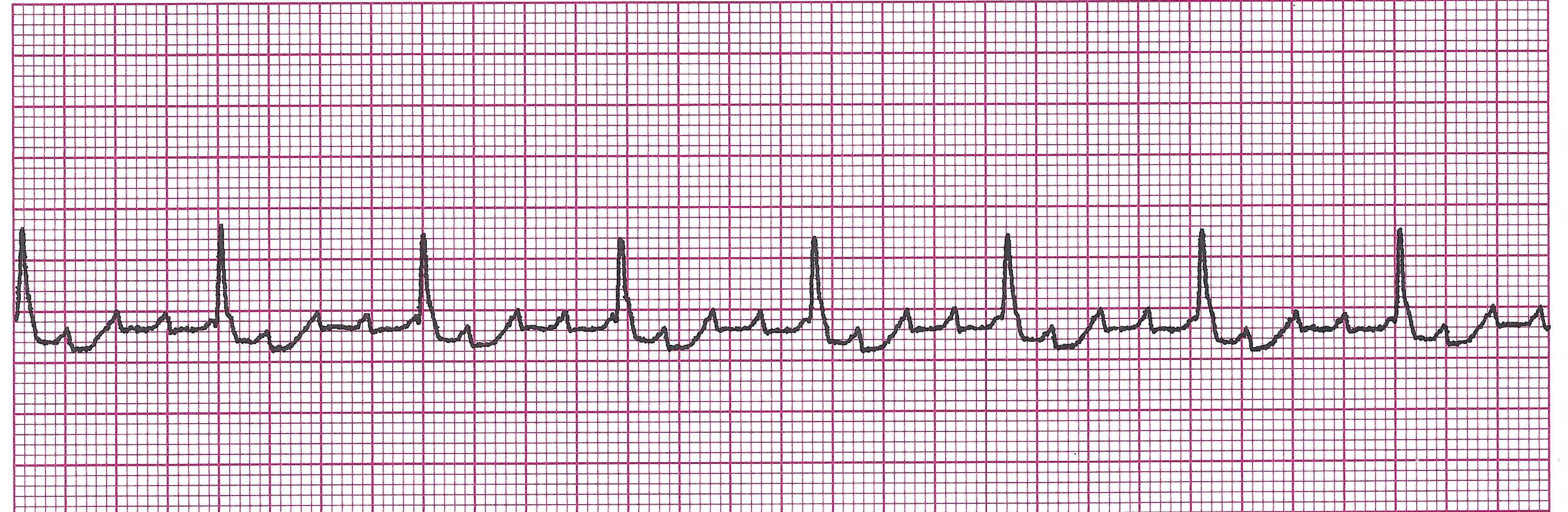
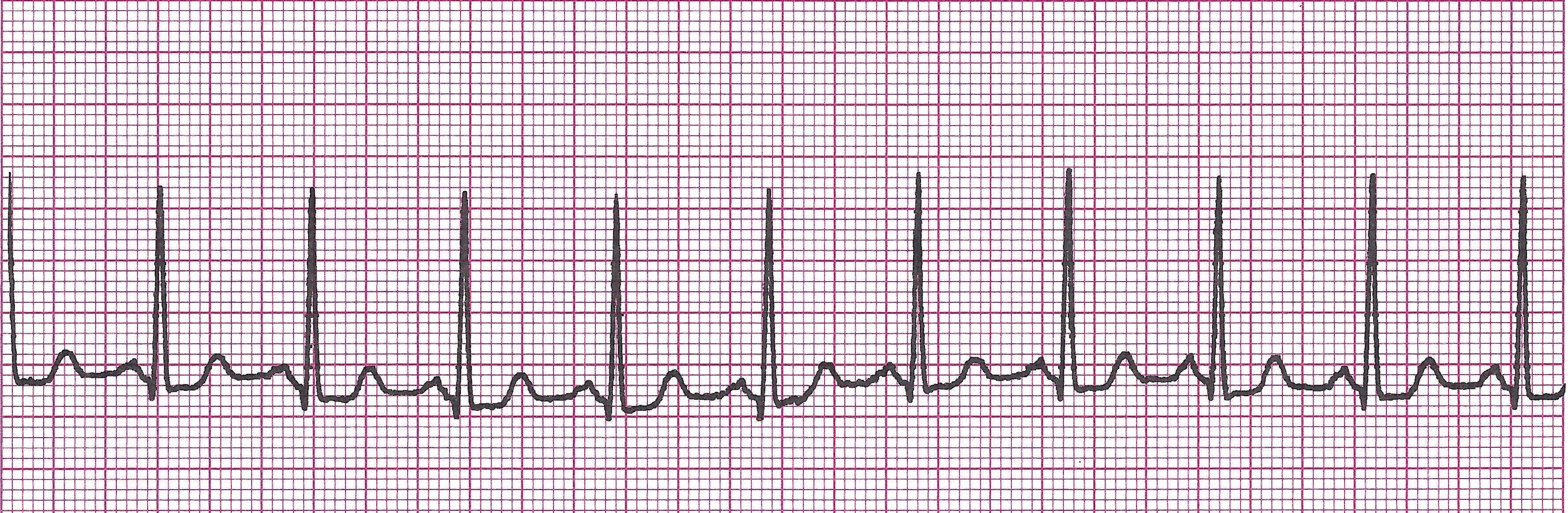
Does each pacer spike capture and get followed by either a P wave or QRS (depending on the type of pacer)?
(In the picture below, there are way more pacer spikes than QRS's, not every pacer spike is followed by a QRS meaning that even though the pacer is firing as programmed, the heart is not responding appropriately.)
· Is the rate reasonable? (Usually 60-100)
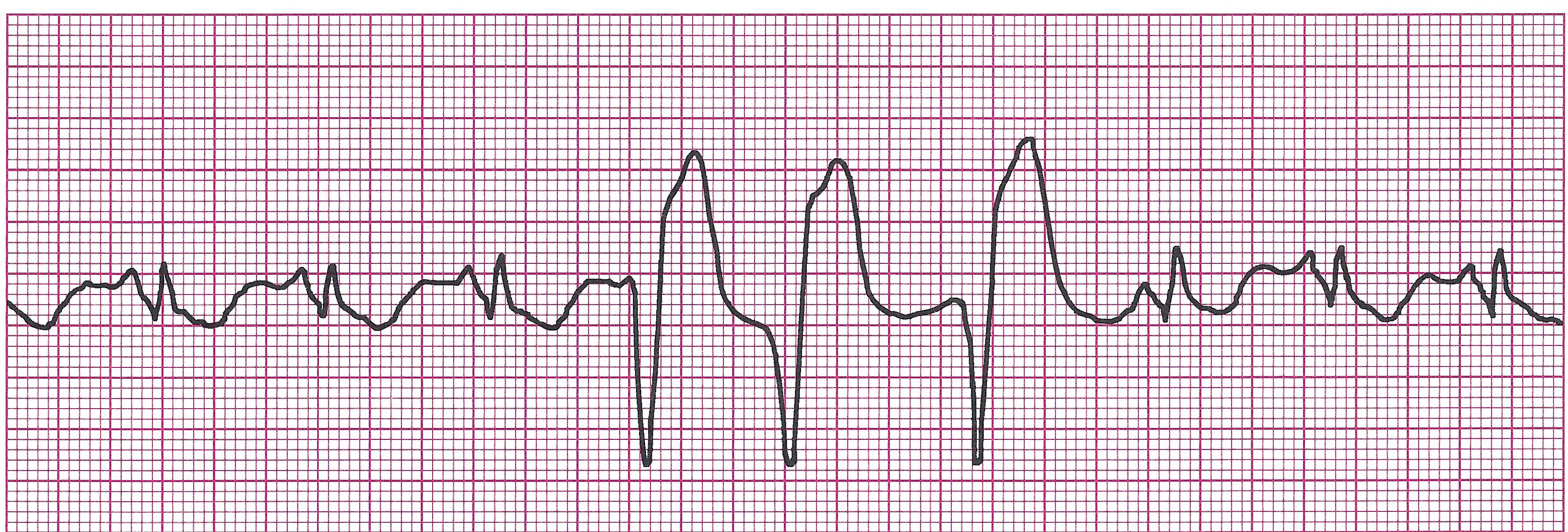
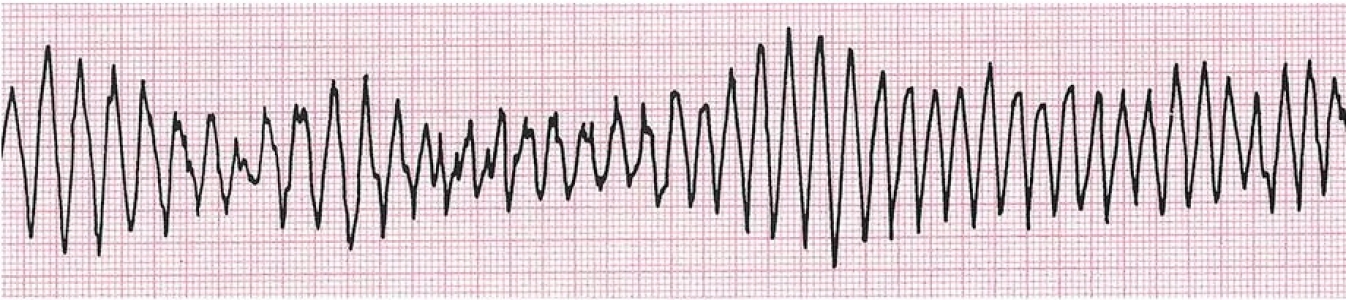
· Are the pacer spikes competing with the patient’s underlying rhythm or falling near T waves? (Spikes falling near T waves can throw a patient into Vtach or Torsades)
· Is pacer firing consistently and reliably?
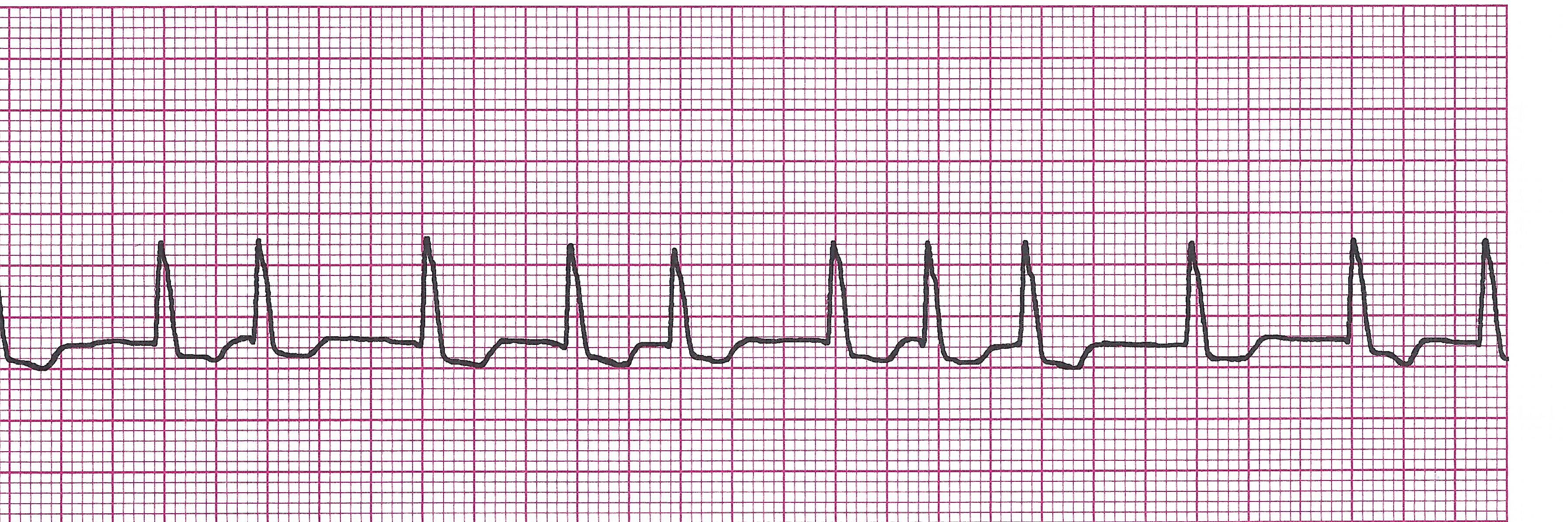
d. Common Malfunctions
1) Failure to Capture- pacer firing, creating pacer spikes, but heart does not respond (no P wave or QRS after)
2) Failure to Pace- Pacer fails to deliver correct number of stimuli or sometimes any stimulus at all.
3) Competing with patient’s own intrinsic rhythm- can be for two reason and either of these can be bad if the depolarized beat falls near the T wave of the previous beat