. Atrioventricular Blocks
a. What are they?
Email : kimberly@avancelearning.com
Contact : 813-508-1511
a. What are they?
These conditions do not come from the AV node. They are a result of an impulse from somewhere above the AV node having trouble getting through the AV junction or the top of the Bundle of His. They are categorized according to the severity of obstruction in the AV junction.
b. First Degree AV block
Example of 1st degree AV block
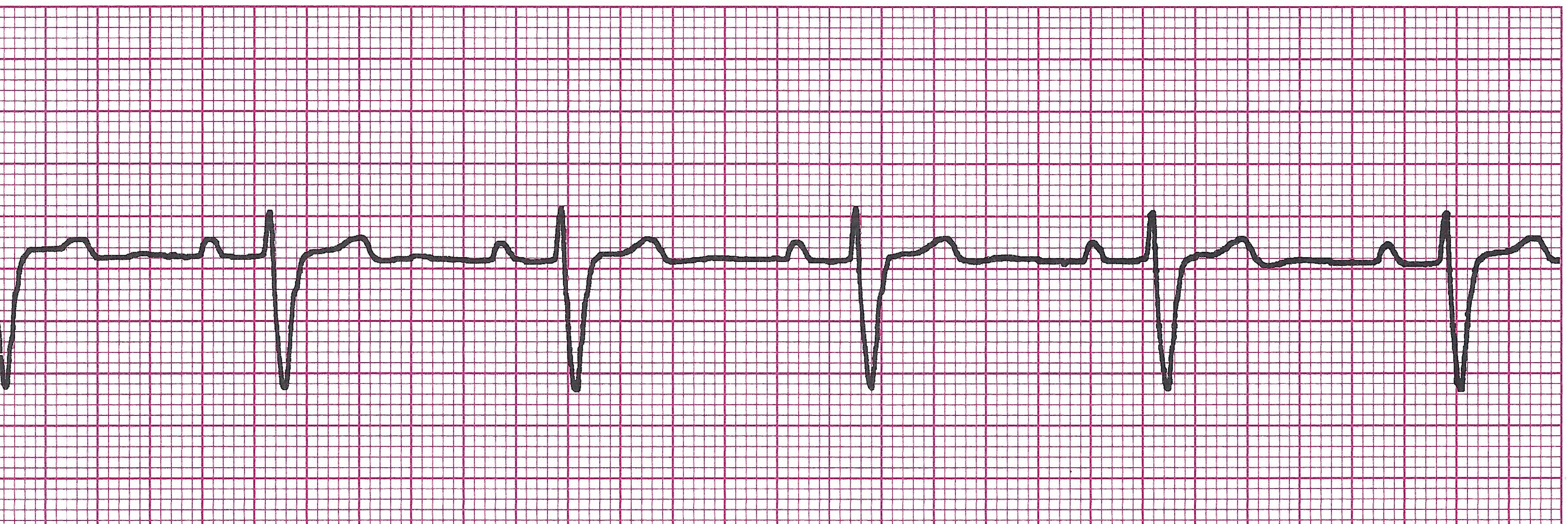
Not a true block because each impulse is conducted. It just takes longer than usual. The block is only partial. It is least serious of all the blocks. REMEMBER: THIS IS NOT A RHYTHM BY ITSELF. IT IS A CONDITION SUPERIMPOSED ON AN EXITING RHYTHM.
· Rules:
Regularity and rate depend on the underlying rhythm
P waves are upright, uniform, and before every QRS
PRI: >0.20sec and constant
QRS: <0.12sec
· Causes: myocarditis, MI, hypothyroid, cardiomyopathies, Digoxin toxicity, anoxia, increased vagal tone, electrolyte imbalances, medication effects like Ca channel blockers, Beta-blockers, cardiac glycosides
· Clinical Picture: Usually asymptomatic, but can lead to a more serious AV block.
· Management: Treat the cause. O2, monitor. Can lead to a more serious AV block.
c. Second Degree AV block MobitzType I (Wenckebach)
Example of 2nd degree AV block Type I (Wenckebach)
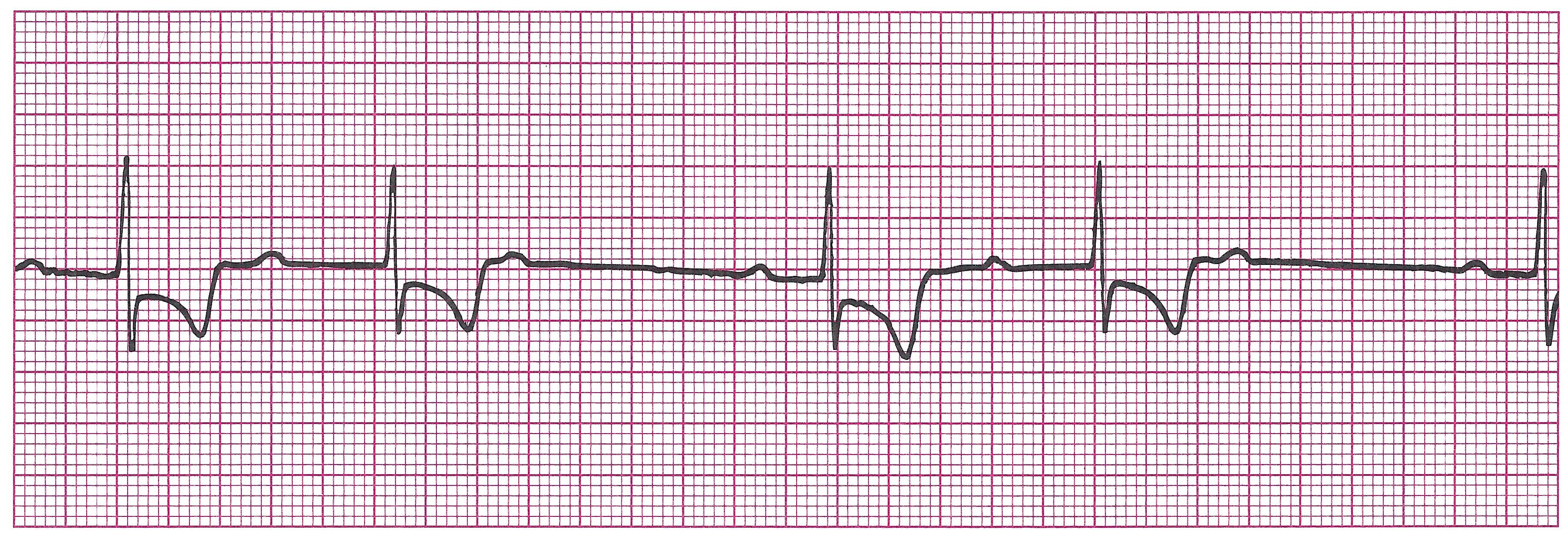
This block is more serious that first degree because not all impulses get conducted through the AV node. The only differences between Second Degree Type I and Type II are the PRI and the number of impulses allowed through the AV node. You will usually see more impulses being conducted with Type I.
· Rules:
Regularly Irregular (Pattern)
Ventricular rate will be slightly slower than usual due to the dropped beat.
P waves upright, uniform, but not always followed by a QRS
PRI gets progressively longer until one P wave is not followed by a QRS (a blocked beat). After this “blocked beat”, the cycle starts again.
QRS: <0.12
· Causes: Medication effects like Digitalis, Beta-blockers, Ca channel blockers, increased parasympathetic tone, myocardial ischemia at or near the AV node, inferior MI
· Clinical Picture: Usually asymptomatic
· Management: Treat the cause. O2. Monitor. Can lead to a more serious AV block. Can also use Atropine, Epinephrine, or transcutaneous pacing if patient becomes unstable.
d. Second Degree AV block Mobitz Type II (Classic)
Example of 2nd degree AV block Type II (Classic)
· Rules:
Regularity may vary depending on how many and which impulses are allowed through. If the conduction ratio is consistent (i.e- every other P wave is not followed by a QRS), then the R-R will be constant and regular. If the conduction ratio varies (i.e. two P waves have QRS then one does not, then one P wave has QRS, etc), the R-R will be irregular.
Ventricular rate will usually be bradycardic due to all the blocked impulses
P waves are upright and uniform. Not all are followed by QRS.
PRI: Constant throughout conducted beats. However, it can be >0.20.
QRS <0.12, however can also be wider depending on the physical location of the block. The lower the block below the AV node, the more likely the QRS will be wider.
· Causes: myocardial ischemia or infarct, myocarditis, Ca channel blockers, Amiodarone, Digoxin
· Clinical Picture: Can by asymptomatic but , if the rate is slow, patient may show signs of decreased cardiac output, SOB, CHF.
· Management: Treat the cause, give O2, establish IV site if patient does not have one already, and MONITOR as this rhythm commonly transitions to complete heart block. Can use Atropine, Epinephrine, and transcutaneous pacing if patient becomes unstable.
e. Third Degree AV block (Complete)
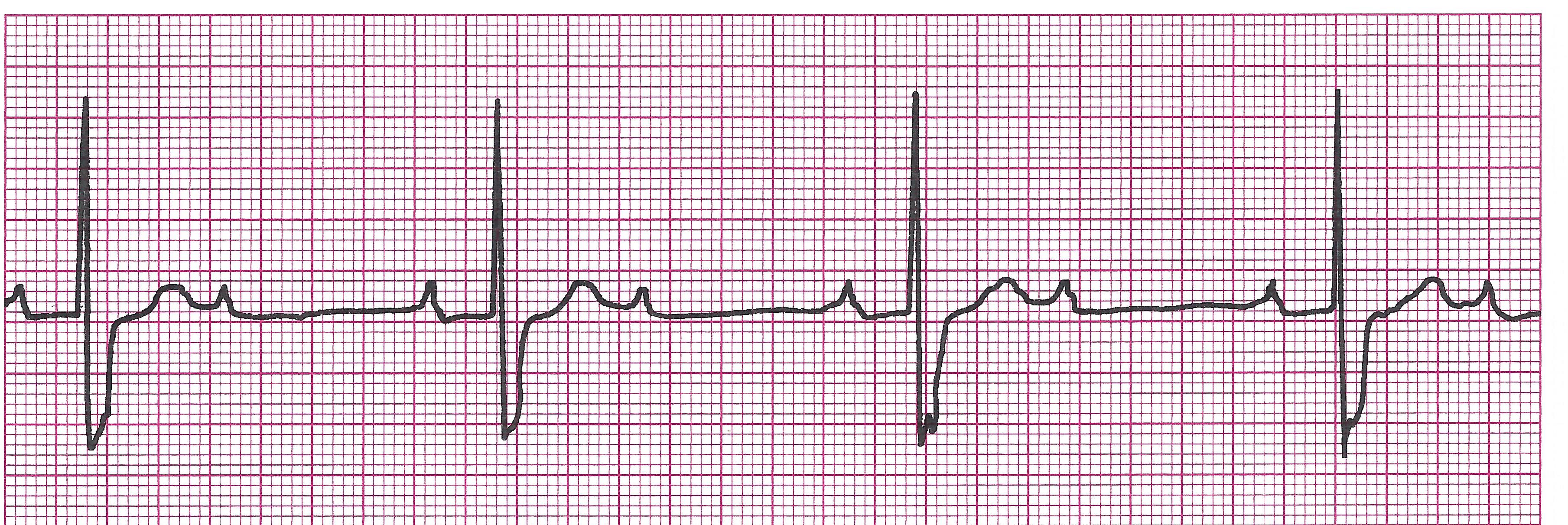
Example of 3rd degree AV block

Third degree heart block occurs when there is a complete block at the AV junction. No impulses conducted from the SA, atria, and sometimes the AV junction can get through to the ventricles. For this reason a lower escape pacemaker (either the lower AV junction or ventricles) kicks in and conducts impulses for the ventricles while the atrial pacemaker (SA, AV node, or atria) conducts impulses for the atria. Because they have different pacemaker sites, the atria and ventricles are beating independently of each other and there is no relationship between the two. Therefore, the contraction of each chamber is not sequenced correctly and the heart cannot fill with blood adequately. Moreover, because the ventricular pacemaker only beats at 20-40bpm, the patient may be very bradycardic and hemodynamically unstable.
· Rules:
P-P intervals and R-R intervals are regular and constant.
Ventricular rate depends on the controlling focus. If junctional: 40-60bpm, if ventricular: 20-40bpm.
P waves will be upright and uniform. Always more P waves than QRS’s and no consistent relationship between P waves and QRS.
PRI: Does not exist since there is no conduction to the ventricles. No relationship exists.
QRS: Depends on the controlling focus. If junctional, QRS will be <0.12, if ventricular, may measure 0.12 or greater.
· Causes: Commonly associated with MI. Other causes include ischemic heart disease, excessive vagal tone, Digoxin toxicity, Ca channel blockers, Beta blockers, electrolyte imbalance, myocarditis.
· Clinical Picture: Usually shows signs and symptoms of low cardiac output. May become unstable.
· Management: Oxygen, Monitor, establish IV site, if patient does not have one. Transcutaneous pacing. Treat the cause, if possible.
STOP! TIME FOR PRACTICE STRIPS ON AV BLOCKS!